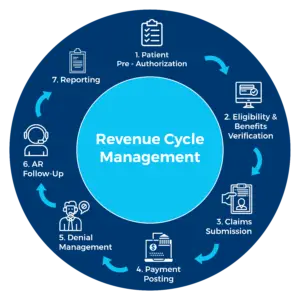
Revenue Cycle Management Services
Our Billers Provide Services Across
These services are backed by years of hands-on experience and daily interactions with both government and commercial payers. Leveraging established relationships, we ensure your practice receives payments faster and more efficiently.
Charge Entry
The Medical billing process begins with filing claims for services provided to patients, entering charges/ creating bills is done electronically to shorten the revenue cycle days.
Patient demographics and medical codes are meticulously verified, ensuring every claim includes accurate information such as DOS, POS, provider details, units, modifiers, CPT codes, billing facility, and referring doctor to minimize the risk of rejection. Your fee schedule is also carefully considered when raising bills.
Our billers submit claims to clearinghouses to maintain 100% accuracy for all clients. Additionally, CMS 1500 forms are generated for submission to government agencies.
We employ a thorough quality process before submitting claims, ensuring a 100% clean claim rate on the first submission. This includes:
- Manual checks by our experienced billers to ensure accuracy.
- Random quality audits using statistical data.

Payment Posting
Payment posting is a crucial step in billing process, looking at the sensitivity of this process, accurate and efficient payment posting process is indispensable for Physicians office. Our billers are known to be highly efficient and analytical in payment posting process.
Our billers understand that reading Explanation of Benefits (EOBs) is a specialized skill requiring deep knowledge of payer communication nuances for effective payment posting management.
They accurately enter:
- Allowed amounts
- Paid amounts
- Patient responsibility information
- Contractual adjustments
This meticulous process simplifies insurance follow-up and ensures precise payment posting.
With the evolution of Electronic Remittance Advice (ERAs), our billers adeptly handle ERA posting, verifying posted payments for accuracy.
Their expertise encompasses advanced electronic remittance scenarios, including denials, underpayments, overpayments, multiple adjustments, automatic cross-over, secondary remittance, reversals, and more.
Before closing the payment posting, our billers ensure patient payments accepted in the front-office match encounters entered in the back-office.
This step-by-step approach to medical billing makes our billers specialists in optimizing your practice’s financial operations.

Accounts Receivable
Money waiting to be collected is revenue loss!
Our billers understand that claim accuracy and efficient payment retrieval are crucial for optimized revenue collections. Our goal is to enhance your cash flow by reducing days in accounts receivable and increasing profitability through an improved collections ratio.
Our billers strategically identify the best category/payer combinations to maximize collections. They prioritize claims by dollar value and date of service, organizing Account Receivables (AR) by timeline (30-45 days, 45-60 days, and beyond 60 days) to address critical claims first.
Skilled in identifying accounts requiring follow-up, our billers take necessary actions to collect unpaid and partially paid claims. They run reports on accounts 21 days past due and contact insurance companies to check claim status, re-file, or gather additional information, maintaining an average account receivable age of 25 days or less.
Many clinics face revenue stagnation due to inadequate insurance follow-up, leaving thousands of dollars uncollected. Our billers minimize tedious hold times with insurance companies by efficiently navigating IVRs.
With years of experience, some of our billers have established relationships and deep understanding of claim statuses, enabling them to follow up without even picking up the phone. They truly know their jobs!

Denial Management and Appeals
Denials are an epidemic to the financial health of most practices, and they have a need to be treated well in order to get you financial success. 10% of the physician revenue is estimated to be lost due to lack of denial management process.
Our billers are experts in denial management analysis, preventing denials and revenue losses before they occur. If you have past denials, our billers and coders can handle them effectively, ensuring they get paid with ease.
The key to successful denial management is thorough analysis. Once the root cause of a denial is identified, correcting it and securing payment becomes straightforward. This requires the expertise of a specialist to achieve precise claim analysis.
Our billers are specially trained to recover collectables from:
- Worker’s compensation
- Medicare
- Medicaid
- Attorneys
Denial claims often necessitate appeals, which involve explaining why a previously denied claim is now eligible for payment. Some appeals are time-sensitive, and our billers review your most commonly denied claims, prioritizing them by volume and dollar value, and file them promptly.
Our billers also consider the cost of appealing claims in terms of time and money, ensuring that appeals are filed strategically. They know that many practices lose significant income annually by not appealing denied claims, and they work to prevent this loss.
By leveraging their skills in denial management, our billers help secure the revenue your practice deserves.
Our billers strategically identify the best category/payer combinations to maximize collections. They prioritize claims by dollar value and date of service, organizing Account Receivables (AR) by timeline (30-45 days, 45-60 days, and beyond 60 days) to address critical claims first.
Skilled in identifying accounts requiring follow-up, our billers take necessary actions to collect unpaid and partially paid claims. They run reports on accounts 21 days past due and contact insurance companies to check claim status, re-file, or gather additional information, maintaining an average account receivable age of 25 days or less.
Many clinics face revenue stagnation due to inadequate insurance follow-up, leaving thousands of dollars uncollected. Our billers minimize tedious hold times with insurance companies by efficiently navigating IVRs.
With years of experience, some of our billers have established relationships and deep understanding of claim statuses, enabling them to follow up without even picking up the phone. They truly know their jobs!

Physician Credentialing
Starting a new practice? Then you definitely need Medical Billers who are experts in setting up practices or getting Physicians credentialed with various payers
Our team of experienced Medical Billers and Coders boasts extensive expertise in physician network introductions and expedited credentialing processes with government agencies.
They possess in-depth knowledge of the credentialing process, including access to key contacts for optimal credentialing offers. Familiar with market offerings of various payers, they negotiate favorable rates for your practice, consulting on fee structures based on community specialist averages and your practice’s unique needs.
Payer Contract Evaluations & Renegotiation: Effective payer contracting, evaluation, and renegotiation are critical for practice success. Yet, many practices overlook regular contract reviews, missing out on potential revenue growth. Our billers facilitate comprehensive contract evaluations and renegotiations, providing quantifiable results that directly impact your bottom line. Reach out via our contact form for prompt assistance.
Annual Credentialing Maintenance: Timely credentialing of Nurse Practitioners and Physician Assistants is essential to avoid revenue loss. Our billers excel in managing this process, allowing you to focus on your practice with confidence.
Medicare Enrollment Services: Our billers navigate the complex Medicare enrollment process efficiently, saving you time and effort. With their expertise, enrolling physicians in the Medicare Program becomes seamless and hassle-free.
Experience the unparalleled level of service you deserve with our dedicated focus on local attention and customer satisfaction.......
We connect practice managers and physicians to specialized medical billing companies. Our network of billing, coding and credentialing providers are actively seeking practices in their target criteria. Ultra Medical Solutions was founded in 2022 by an experienced internet marketing team.
Services
Copyright © 2024| Powered by ultramedicalsolutions.com

